A tiny wire made a huge difference in young Amanda Rosengren’s quality of life, giving her the type of security, safety, and freedom every teenager needs.
At first glance Amanda Rosengren looks just like any other teenager: she loves hanging out with her friends, competing in sports and dreams about a career in acting. Oh, and she’s constantly on her smartphone. But, if you look a bit closer, Amanda checks her phone a bit more carefully than the other kids.
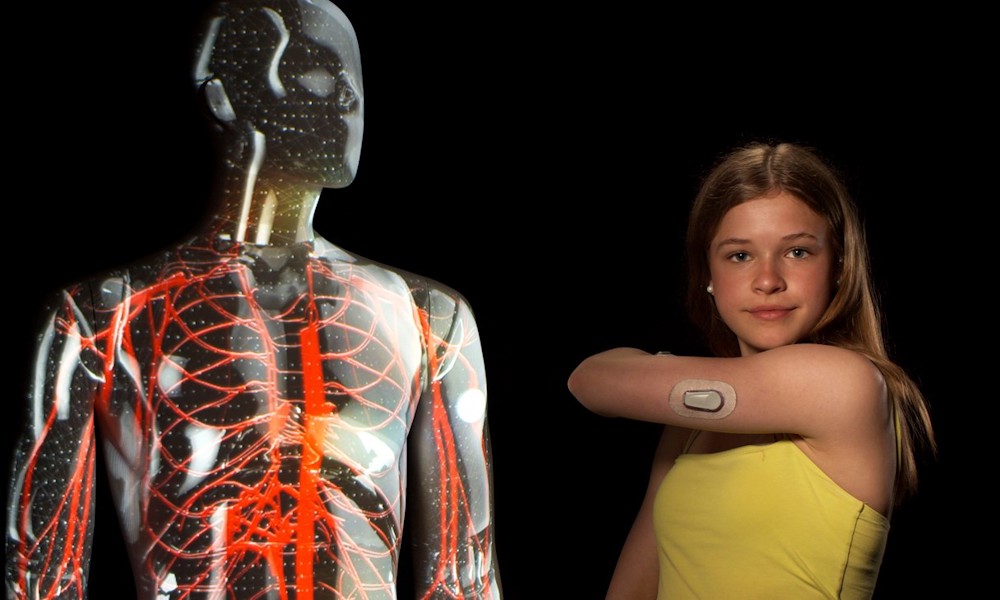
Amanda’s smartphone is actually a lifesaving tool. It is where her blood sugar level is shown with the help from a CGM (continuous glucose monitor). A tiny medical wire is inserted under the skin in one of her arms and it functions as a sensor that sends information to an app in her smartphone. The CGM is one of the applications that medical wire from Alleima is used in. The wire is so tiny that it has been used in insect brains to test responses to stimuli. The small size and the high quality of the wire makes it ideal for use in medical devices that are implanted inside humans.
Checking her blood sugar levels is a routine part of her daily life. Amanda has type 1 diabetes, a never-ending disease that can be very dangerous if blood sugar levels are not constantly monitored and adjusted with insulin.
I wasn’t allowed to go too far away from home. If I went out, I got loads of phone calls from mum and dad.

Now 13 years old, Amanda is used to her condition and its challenges – she was only four when she and her family found out about her condition, so she has basically grown up a diabetic. Actually, she still remembers the day back in 2011 when one of her teachers at kindergarten alarmed her parents that something wasn’t quite all right, that Amanda acted differently than the other kids. She was very thirsty and went more often to the bathroom. On top of that Amanda, who normally was very tired when the kids had their daily nap, now didn’t seem to be able to fall asleep at all.
“Since my teacher had diabetes herself, she understood that these things could be symptoms of the disease and called my parents,” Amanda says.
Amanda remembers her dad showing up earlier that day to pick her up from kindergarten. After a urine test at the emergency room, Amanda was diagnosed with diabetes. The family had to stay at the hospital for a week after getting the diagnosis. They met a therapist and a dietician and Amanda’s parents were trained in how to treat a diabetic child.
After that turbulent week, the family moved back home to a host of changes. Needles, blood samples and blood sugar controls became a daily necessity. Since diabetes is a serious illness, Amanda’s parents were obviously worried constantly and tested her blood sugar frequently. At this point Amanda was full of needle marks on her hands and arms.
A very limiting time
Constantly monitoring the blood sugar levels of a diabetic is a never-ending dance between eating and insulin injections to keep the blood sugar at a steady level. When it comes to children, the care needs to be individually adjusted since each person is unique. Amanda’s blood sugar levels were pretty difficult to monitor, since they often fluctuated, which put even more pressure on Amanda’s family. Her parents were afraid to leave her alone and slept and worked in shift. They also found it hard to let Amanda go to kindergarten, even though they got an extra daily resource to help her there. This went on for years.
Amanda remembers this time as very limiting to her and that she was treated differently than her friends.
“I wasn’t allowed to go too far away from home,” she says. “If I went out, I got loads of phone calls from mum and dad, who of course were worried about me. And when my friends had sleepovers, my parents came to pick me up when it was bedtime.”
But in 2013 Amanda’s mother Helen Blomqvist, who is a bit of a tech geek, heard about the CGM that measures tissue glucose 24 hours a day. This means that you can immediately view your glucose value, a trend graph and in particular the direction the value is going in.
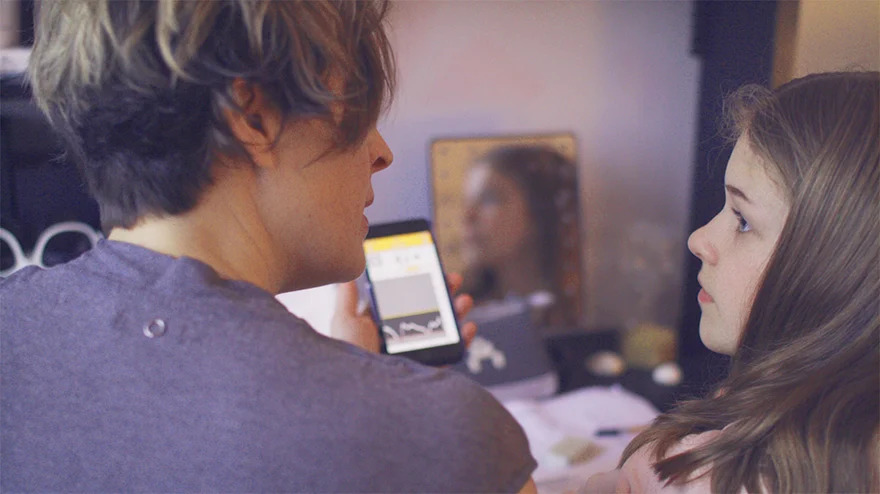
In March 2014, Amanda’s medical diabetic team suggested that the family should test the CGM. Today, she gets readings on her blood sugar level and that information is sent in real time to an app on her smartphone. If her blood sugar level is going high or low, she instantly gets a warning.
Amanda also has an insulin pump attached to her stomach, that automatically gives her the right dose of insulin according to the measurements the app recommends.
The new technique has provided Amanda and her family a new lease on life. Since Amanda’s blood levels are constantly monitored and registered in the app, the family can be more spontaneous.
“Seeing the blood sugar levels visually is very powerful, you really do know if you have a high or low value,” says Helen Blomqvist, Amanda’s mother. “It makes us and Amanda feel very safe. This technique means everything to us.”
And with the alarm function that is integrated in the system, her parents can sleep better – knowing they will wake up by an alarm in case Amanda gets a too high or low blood sugar level.
Facts Diabetes
Around 415 million people live with diabetes, roughly nine percent of the world's adult population.
46 percent of people with diabetes are undiagnosed.
China, India and the US are the top three countries where diabetes is most prevalent.
Approximately eight percent of people with diabetes have Type 1 diabetes, versus 92 percent who live with Type 2.
Type 1 diabetes can appear at any time in someone’s life after the destruction of pancreas cells, which produce insulin. This is known as insulin-dependent diabetes, which many manage by injecting insulin themselves or using an insulin pump.
Type 2 diabetes develops when the body becomes resistant to insulin or when the pancreas is unable to produce enough insulin. This is usually a result of genetic or environmental factors, such as weight.
A continuous glucose monitor (CGM) replaces the need for the pin-prick insulin testing method in Type 1 diabetes. A CGM measures glucose tissue 24 hours a day, and a tiny wire implanted under the skin acts as the CGM’s sensor.
About the wire
Precision medical wire from Alleima provides solutions for continuous glucose monitoring to assist diabetic patients manage their disease.
The glucose levels are gathered via a chemical reaction from the wire sensor inserted under the skin which transforms to electrical signals sent to a transmitter outside the body.
Today you can view your glucose levels in real-time in your smartphone app.
Wires of this kind can also be found in other applications such as consumer micro-electronics.
Alleima wire can be made using an extensive range of stainless steels, precious metals and other biocompatible alloys, such as cobalt-chromium alloys.